High body fat from childhood was not associated with progressive vascular damage in young adulthood, a paper published in Hypertension Research concludes. The researchers examined cumulative exposure to high-fat mass over a period of 15 years.
We are inundated daily with information regarding the negative effect of body fat on cardiovascular health. Weight-to-height-based indirect measures of obesity such as body mass index (BMI) have been key indicators for recommending weight control regimens, even in growing children and adolescents. Thus, slim body size may become a target and sometimes even an obsession already in early life. Even parents are sometimes discouraged at the weight of their children simply based on BMI measures when otherwise the kids are healthy.
The current study showed that we cannot rely on BMI in early life because most of the weight described by BMI is muscle mass and not fat mass. In this study, muscle mass and fat mass were measured in over 3800 participants with dual-energy Xray absorptiometry (DEXA) scanners during a 15-year follow-up period. Children had approximately four-fold more muscle mass than fat mass at age 9 years. This muscle-to-fat mass ratio remained the same until 17 years of age and slightly decreased to three-fold more muscle mass than fat mass by age 24 years among BMI-categorized normal weight 3100 participants. However, among the BMI-categorized overweight and obese 730 participants, the muscle-to-fat mass ratio was 2.3 at 9 years, 1.7 at 17 years, and 1.69 at 24 years of age.
It is important to note that fat mass tripled in both males and females over 15 years while muscle mass doubled in the whole cohort. However, this increase in fat mass seems physiologic and healthy due to the balance with increasing muscle mass and was not associated with measures of sub-clinical atherosclerotic cardiovascular disease in the study.
“Since BMI does not directly measure fat mass and muscle mass, previous associations between increased BMI and vascular function have been erroneously adjudged an adverse effect of fat. Therefore, encouraging young people to lose weight may imply a recommendation to decrease muscle mass, leading to a low muscle-to-fat mass ratio,” says Andrew Agbaje, a physician and clinical epidemiologist at the University of Eastern Finland.
In this study, increasing muscle mass was associated with optimal vascular health, especially in males. In adults, studies have shown that lower muscle mass may lead to cardiovascular diseases, musculoskeletal diseases, and cancer. Therefore, it is important to gain adequate muscle mass from childhood through young adulthood which would enhance healthy vascular function and development.
“A functional and healthy artery may promote better cardiovascular health in later life. Therefore, practices like extreme obsession with weight loss and severe food restriction should be discouraged in youths because it may negatively alter vascular function and subsequently lead to cardiovascular disease in later life.”
“Nonetheless, this study does not justify an excessive weight gain that alters the balance of optimal muscle and fat mass ratio. Excessive weight gain or low muscle-to-fat mass ratio should be avoided because evidence shows that severe and morbid obesity is a risk factor for several diseases.”
“In a nutshell, weight gain from childhood through young adulthood is not always bad for cardiovascular health. It may be a good sign of healthy muscle building which enhances the heart and vessels to pump blood and oxygen efficiently. A four-fold increase in muscle mass compared to fat mass from early life is key to better vascular health, thus parents, caregivers, pediatricians, public health practitioners, and health guidelines should aim at a ‘muscle mass (MM) X 4 to fat mass (FM) X 1’ ratio target, simply abbreviated as MM4–FM1” Agbaje says.
“It is worth noting that it wasn’t easy or quick to get this paper published, due to the controversial nature of the results. Some reviewers’ comments were downright hostile toward these results which seem to challenge the existing paradigm. However, science is improved with better measurement, study design, and advanced analytical technique, and scientists should aim at constructive critique, objectivity, and flexibility towards a paradigm shift,” says Andrew Agbaje.
Dr Agbaje’s research group (urFIT-CHILD) is supported by research grants from Jenny and Antti Wihuri Foundation, the Finnish Cultural Foundation Central Fund, the Finnish Cultural Foundation North Savo Regional Fund, the Orion Research Foundation sr, the Aarne Koskelo Foundation, the Antti and Tyyne Soininen Foundation, the Paulo Foundation, the Yrjö Jahnsson Foundation, the Paavo Nurmi Foundation, the Finnish Foundation for Cardiovascular Research and the Foundation for Pediatric Research.
For further information, please contact:
Andrew Agbaje, MD, MPH, Cert. Clinical Research (Harvard), Principal Investigator (urFIT-CHILD). Institute of Public Health and Clinical Nutrition, School of Medicine, University of Eastern Finland, Kuopio, Finland. [email protected], +358 46 896 5633
https://uefconnect.uef.fi/en/person/andrew.agbaje/
Link to the article:
Agbaje AO, Barker AR, Tuomainen T-P. Cumulative muscle mass and blood pressure but not fat mass drives arterial stiffness and carotid intima-media thickness progression in the young population and is unrelated to vascular organ damage. Hypertens Res 2022. https://www.nature.com/articles/s41440-022-01065-1
Webpage:
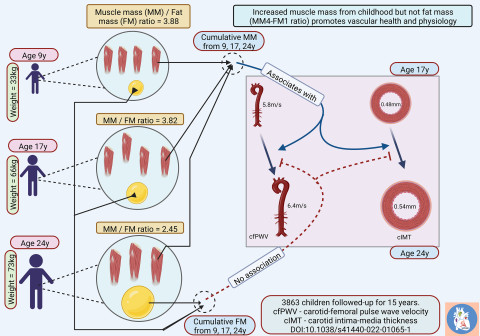
During growth from childhood (9 years) to young adulthood (24 years), body fat mass tripled as children gained weight. However, this increase in body fat was not associated with signs of subclinical atherosclerosis progression likely due to the significant increase in muscle mass. A muscle mass-to-fat mass ratio of 4:1 (MM4-FM1) may promote excellent vascular health from childhood. Image: Andrew Agbaje.



