You, too, could be suffering from fatty liver – even if you don’t drink any alcohol. Often, weight gain causes fat to build up in the liver, but also genes, gut microbes, and even environmental chemicals play a role.
One in four adults has fatty liver, which means that excess fat has accumulated in their liver cells, and the accumulation of fat in the liver has been observed even in children. Fatty liver is a lifestyle disease, and the risk for developing one is increased by overweight and a lack of physical exercise. Diet quality plays a role, too. Eating too much sugar, low-fibre grains and foods rich in hard fats, such as butter and high-fat dairy products, speeds up the accumulation of fat in liver cells. Heavy drinking is also a considerable risk factor; however, only one in five cases of fatty liver disease is caused by alcohol.
“The false idea of fatty liver being exclusively an alcohol induced disease is perhaps the reason why it isn’t talked about much. However, it is a major public health issue,” Professor of Nutrition Therapy Ursula Schwab from the University of Eastern Finland says.
Last year, the treatment of non-alcoholic fatty liver disease was introduced in the Finnish Current Care Guidelines as a disease of its own, and Professor Schwab was involved in the working group drafting the guidelines.
Fatty liver is often part of a wider metabolic disorder. It is common in people who display characteristics of metabolic syndrome, such as abdominal obesity, high blood pressure and abnormal blood glucose and fat levels. As many as 60–70% of people with type 2 diabetes also have fatty liver. However, skinny people, too, can develop fatty liver, and not everyone who is overweight gets it.
The liver fat concentration can be reduced even by moderate weight loss.
Weight loss reduces fat from the liver, too
There is no medication specifically for fatty liver disease. The primary treatment is to lose excess weight, exercise more and follow a healthy diet; one that favours sources of soft fats, such as vegetable oils and fatty fish, and avoids sugary drinks. Regardless of the cause of the disease, fatty liver is easily damaged by alcohol, which means that its consumption should be restricted.
A high intake of fructose, or fruit sugar, has been associated with fatty liver but according to Professor Schwab, this does not mean that fruit should be avoided. A glass of 100% fruit juice a day is okay, too.
“In Finland, an excessive intake of fructose is rarely a problem. However, in the US, for example, many drinks are sweetened with high fructose corn syrup, and consumption of these kinds of drinks can easily lead to a high intake.”
It is important to treat fatty liver before it leads to irreversible liver injury or even liver cancer. Fatty liver used to be considered a relatively harmless condition, but in some people, the disease progresses to liver inflammation and liver fibrosis, where scarring connective tissue is formed in the liver, and ultimately to liver cirrhosis, where scarring leads to liver failure. At the same time, the risk of liver cancer also increases.
“The liver fat concentration can be reduced even by moderate weight loss. In cases where connective tissue has already formed in the liver, lifestyle changes can still promote the health of the remaining liver tissue.”
“In the hospital, we unfortunately see cancer patients whose liver cancer probably could have been prevented if their fatty liver disease had been treated in time. Fatty liver can be easily missed in people who are normal-weight and physically active. In most cases, of course, the disease is associated with overweight,” Professor Schwab says.
The idea is to examine whether physical exercise changes the microbiota so that the accumulation of fat in the liver decreases.

Exercise and dietary changes may affect the liver via gut microbes
Genetic susceptibility to fatty liver disease may partly explain the development and individual progression of the disease. The risk of fat accumulating in liver cells is increased, for example, by the PNPLA3 gene variant, which as many as 40% of Finns have inherited from at least one parent.
In recent years, it has been observed that fatty liver disease also involves changes in the gut microbiota. Funded by the EU, the BestTreat research consortium is currently investigating how the microbial composition of the gut affects the prognosis of the disease, and whether it could also be treated by promoting a normal composition and function of the gut microbiota. As a member of this European consortium, Professor Schwab's research group seeks to find out how physical exercise affects the microbial composition of the gut and the accumulation of fat in the liver.
“The idea is to examine whether physical exercise changes the microbiota so that the accumulation of fat in the liver decreases.”
People diagnosed with non-alcoholic fatty liver disease participated in a 12-week exercise programme. The programme included one weekly exercise session of the participants’ own choice, such as walking, jogging or swimming, and two supervised exercise sessions on a bicycle ergometer, with resistance increasing in tandem with fitness.
“Three months should be enough to achieve clinically relevant results. However, these findings are yet to be published, because they will be combined with data from a similar intervention in the Netherlands next winter,” Professor Schwab says.
Professor Schwab’s research group is currently conducting another study to investigate the association between dietary fat quality and the accumulation of fat in the liver. Half of the study participants have inherited the PNPLA3 risk variant from both parents, while the other half are not variant carriers.
“Other studies have shown us that by making lifestyle changes, it is possible to silence genes that make people susceptible to diseases. Now we will see if this gene can be silenced by replacing saturated fats with unsaturated ones, as encouraged in nutrition recommendations.”
The effects of dietary changes will be examined not only on the participants’ liver tissue, liver enzymes and glucose tolerance, but also on their gut microbiota.
“The effect of the diet on the gut microbiota, and further on the accumulation of fat in the liver, is not yet fully understood, although a link between them has been observed.”
The gut and the liver are in constant interaction with one another through, for example, compounds produced by gut bacteria.
Researchers identified gut bacteria associated with the progression of fatty liver disease
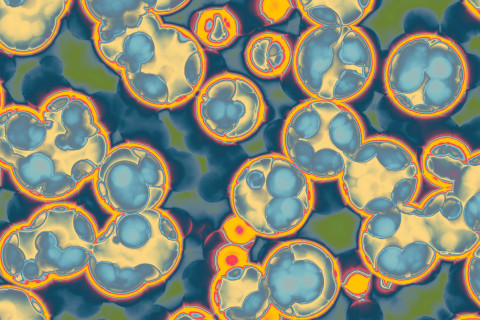
Our gut is home to bacteria that are both beneficial and harmful to health.
“Harmful gut bacteria are also needed because they play a role in training the immune system to function normally. However, it is important that there is a balance between good and bad bacteria,” says Professor of Gut Health and Food Safety Hani El-Nezami from the University of Eastern Finland.
For instance, a high intake of saturated fats, alcohol or antibiotics may throw the gut microbiota off balance and thus open the door to the development of fatty liver disease, and many other diseases, as well.
The gut and the liver are in constant interaction with one another through, for example, compounds produced by gut bacteria. If harmful gut bacteria are able to take over, this may increase intestinal permeability and allow bacterial products that promote inflammation and cell damage to enter the liver.
Professor El-Nezami also holds a professorship at the University of Hong Kong and has, together with international collaborators, identified bacterial clusters that are associated with the development and progression of non-alcoholic fatty liver disease, all the way to liver cirrhosis and liver cancer. These bacteria are found in the gut of people with fatty liver disease, but not in the gut of healthy people.
“This may enable the disease to be prevented or its progression stopped by microbial therapy, which is used to reduce these harmful bacteria.”
Indeed, the research group has already developed a probiotic product for fatty liver disease, and a patent is pending.
“We are talking about third-generation probiotics. Their effect is based not only on the modification of gut bacteria, but also on the compounds released by them.”
“Microbial therapy is a novel concept, but it is a carefully targeted form of treatment. Its efficacy and safety will be demonstrated in animal tests and clinical trials. However, microbial therapy is not an alternative to lifestyle changes, but hopefully can supplement them in the future treatment of fatty liver disease.”
Some chemicals found in our environment are known as metabolic disruptors that affect glucose and fat metabolism.

Environmental chemicals may promote the accumulation of fat in the liver
Recent studies show that the chemicals we get exposed to in our everyday life may also contribute to the development of fatty liver. Many chemicals found in our environment are known to interfere with the normal function of hormones. Some of these endocrine disruptors are known as metabolic disruptors that affect glucose and fat metabolism.
“In the light of recent research, it seems that chemicals can contribute to the development of fatty liver, especially if also other factors that make a person susceptible are at play,” Project Researcher Sini Pitkänen says.
Some examples of metabolic disruptors include plasticisers, pesticides and substances released from industry to the environment, such as dioxin, the main source of which for Finns is fish from the Baltic Sea.
“However, metabolic disruption is still a relatively new topic for research because so far, endocrine disruption in the context of chemical risk assessment has mainly been examined from the perspective of reproductive hormones. There are few methods in place to systematically measure the capability of chemicals to disrupt metabolism.”
She is involved in developing such risk assessment methods in the EDCMET project funded by the EU.
“If we think about the development of fatty liver, metabolic disruptors can contribute to it in a number of ways. For example, they can activate nuclear receptors that regulate fat metabolism in cells and increase the accumulation of fat in liver cells. They can also increase oxidative stress, which depletes cellular resources and reduces the ability of cells to react to environmental stimuli.”
The group is currently developing methods for measuring specifically these effects.
“Methods are first tested with known metabolic disruptors and their reliability is also validated by testing them in partner laboratories in different countries.”
“The chemicals we currently focus on are plasticisers that may enter food from plastic packaging and bottles.”
Fatty liver may be found by accident – people with type 2 diabetes need regular assessment
What are we talking about?
- Fatty liver is the most common liver disease.
- In fatty liver disease, the fat content of the liver exceeds five per cent.
- Most of the cases are non-alcoholic fatty liver disease, NAFLD. The advanced form of the disease, non-alcoholic steatohepatitis, NASH, is associated with liver inflammation and the replacement of healthy liver tissue with connective tissue, i.e., fibrosis, which can progress into irreversible liver cirrhosis.
- Fatty liver disease is the main cause of hepatocellular cancer.
- Advanced fatty liver disease increases the risk of cardiovascular diseases.
- In people with type 2 diabetes, fatty liver may make it difficult to achieve a good therapeutic balance.
How is it treated?
- Fatty liver disease is treated through weight loss, lifestyle changes and effective treatment of metabolic syndrome. There are no specific medicines for the disease, but pharmacological therapy with e.g. weight loss medicines or diabetes medicines, bariatric surgery and liver transplantation may be considered in the advanced stages of the disease.
How is it diagnosed?
- Fatty liver is usually asymptomatic. Often, it is found when examining a patient’s abnormal liver enzyme levels (ALT and AST), or as an incidental finding of a radiological examination.
- Although an elevated level of ALT may be indicative of fatty liver, half of patients with fatty liver disease have normal ALT levels.
- Fatty liver is common in patients with metabolic syndrome or type 2 diabetes. According to the Finnish Current Care Guidelines, patients whose fatty liver disease has progressed should be identified from among these patients.
- For people with type 2 diabetes, the risk of fibrosis should be assessed every two years using risk calculators (FIB-4 and NHS). If the result indicates a high risk, advanced fibrosis can be diagnosed with ultrasound-based elastography. Early fibrosis and inflammation can be diagnosed from a biopsy, when necessary.
- In patients who have metabolic syndrome but no diabetes, an elevated ALT level gives cause to assess the risk of fibrosis.
Sources:
Non-alcoholic fatty liver disease (NAFLD). Current Care Summary. Published 08.01.2020.Working group appointed by the Finnish Medical Society Duodecim and the Finnish Association for General Practice.
Fatty liver - what to do? English summary in Männistö, V. & Pihlajamäki, J. Rasvamaksa - entä sitten? Duodecim 2016;132(18):1707-13.
Diagnosis of non-alcoholic fatty liver disease (NAFLD). English summary in Yki-Järvinen, H. Alkoholiin liittymättömän rasvamaksataudin (NAFLD) diagnoosi. Duodecim 2016;132(22):2099-106.